What To Do When You Get Billed Twice By Health Services
Understanding Medical Bills
Medical billing in the United states of america can seem like an extremely convoluted process. According to a 2016 public opinion survey conducted by Copatient, around 72% of American consumers are confused by their medical bills, and 94% of consumers have received medical bills they considered to be "too expensive". Even when covered by insurance or Medicare, you may observe unexpected balances due to odd procedural codes, a slew of medical jargon, and insurance adjustments.
This guide volition help you, as a patient, navigate the medical billing process from the moment you contact a healthcare provider about an appointment until afterward you receive your bill in the post. We hash out how healthcare providers decide costs and negotiate charges with your insurance provider. Finally, we show you how to identify and dispute erroneous charges on your bill.
What Medical Bills Really Cover
Fees might seem arbitrary when you lot enquire for cost estimates from your insurer or when y'all receive a bill after your date. However, there are several elements that factor into how hospitals, physicians' offices, and other institutions calculate the toll of wellness services. If possible, contact your insurer to get toll estimates for multiple healthcare providers in your area. You may discover fees vary quite a scrap for the aforementioned services.
In a New York Times op-ed entitled "Why Medical Bills Are a Mystery," professors Robert Kaplan and Michael Porter of Harvard Business School explicate that providers "assign costs to patients based on what they charge, not on the bodily costs of the resources, similar personnel and equipment used to care for the patient." Here are the considerations medical offices and hospitals make as they negotiate with insurance companies virtually the costs that appear on your bill:
- Facility capacity: Hospital capacity growth is a factor that the National Institute for Health Care Management (NIHCM) Foundation watches closely, since the number of beds in a hospital can dramatically influence what hospitals accuse under a fee-for-service (FFS) system. As hospitals add more than beds, they have a greater opportunity to provide certain medical services. As the NIHCM notes, "Higher system capacity tin lead to competition among suppliers and downward pressure on prices."
- Supply and demand: How readily available are the services you lot need? Are there multiple loftier chapters hospitals or physicians' offices in your surface area that tin provide this service, or do you just have admission to a limited number of specialists? Dr. Robert Stonebraker explains in his open up source book, The Joy of Economic science, "Firms facing little or no competitive pressure are free to raise prices well above the true price of service. Monopoly power drives upwards prices in medical care, just as it would it in retailing and restaurants."
- Hospital reputation: A infirmary'south reputation has a ripple upshot on how many patients use a facility, which in turn influences demand and price. However, the Agency for Healthcare Research and Quality warns consumers that "Clinical quality scores contributed fiddling to hospital choice compared with a infirmary's reputation." This tin can drive business and influence service costs, but yous shouldn't rely on perceived reputation every bit an indication of functioning and quality.
- Charge Description Master (CDM) lists: This resource is a master list of service costs and billing identifier codes that medical billing professionals use during the claims process every bit health offices calculate how much to bill insurance companies and patients. Each hospital maintains its own individual chargemaster list. The American Wellness Information Management Association (AHIMA) recommends that CDM prices should be maintained by chargemaster committees that oversee responsibilities like "reviewing all charge dollar amounts for appropriateness by payer."
Medical billing and coding professionals are working behind the scenes from the moment yous schedule an engagement upwardly until you receive a bill. Most patients aren't familiar with the negotiations that occur between insurance companies and healthcare providers. Understanding the dorsum and along can take some of the mystery out of the insurance and billing processes.
How the Billing Wheel Works
- You contact a healthcare provider. Pre-register and provide basic information to the office, such equally identification and insurance information. You schedule an appointment.
- Information technology is important to inquire the healthcare provider nigh the services and supplies y'all'll receive. If you are not clear on upcoming charges or what insurance will cover for the appointment, then be sure to enquire for the procedure codes.
- Next, contact your insurance company to find out if these services are covered by your program. If and then, get an estimate of how much the services toll with your health insurance.
- If the cost is not manageable, ask your insurer if at that place are other healthcare providers in your area who provide the same service for less.
- The healthcare provider contacts your insurance company in order to verify:
- Preauthorization: Some insurance companies require prior authorization before they cover a medical service or medication. The insurance company collects further information regarding your appointment and medical records before determining whether the services and medications are covered.
- Co-Pay: The healthcare provider'southward office also determines how much the patient must pay out-of-pocket for this visit.
- On the day of the engagement, you complete whatsoever additional registration paperwork, supplying your insurance card, a valid ID, policyholder name, and your insurance grouping number. This registration process helps healthcare providers:
- Update your medical records electronically; pre-existing conditions can factor into coverage decisions
- Provide you with privacy policy information
- Gain your consent to perform certain procedures
- Inform y'all of care liability and risks
- Inform you of patient financial responsibilities
- Determine your advanced directive preferences, which will give healthcare providers articulate instructions if you are unable to speak for yourself
- After services are received medical coders identify all services, prescriptions, and supplies received during your appointment and update your records with the respective service codes.
- The healthcare provider creates an insurance claim using these codes. They then submit an 837 file to your insurance, the standard file format set by the Wellness Insurance Portability and Accountability Act (HIPAA), assuasive your healthcare provider to communicate securely with your insurance.
- A claims processor, who works for your insurance provider, reviews the insurance claim and verifies that the treatments y'all've received autumn nether your coverage benefits. (At this signal, the insurance claims processor may contact you or your healthcare provider for boosted information regarding the services and/or supplies yous received.) The insurance claims processor decides whether the merits is valid, then accepts or rejects information technology.
- The insurance claims processor contacts your healthcare provider with the status decision. If the claim is valid, insurance reimburses your healthcare provider by paying for some or all of the services. If rejected, the claims processor provides the billing role with a detailed clarification of why the services are not covered.
- Your healthcare provider bills you for the remaining residual.
Note: If you are 65 or older, yous are entitled to federal health benefits through Medicare. This social insurance programme differs significantly from individual health insurance providers when it comes to billing. Rather than negotiating prices with a healthcare provider like individual wellness insurers, Medicare publishes prepare fees for services. If yous are enrolled in Medicare Part B, your healthcare provider consults the Medicare Physician Fee Schedule (MPFS) to determine the set price for the services you received.
How to Read Your Bill
Once you receive a medical bill from your healthcare provider, you lot will notice that information technology consists of multiple components that might non be clear to you. For most patients, the codes, descriptions, and prices listed in their bills can seem disruptive.
The following instance explains each element of your neb with an in-depth description. Information technology is important non to get your medical bill confused with the Explanation of Benefits (EOB), an insurance report nosotros encompass following the nib.
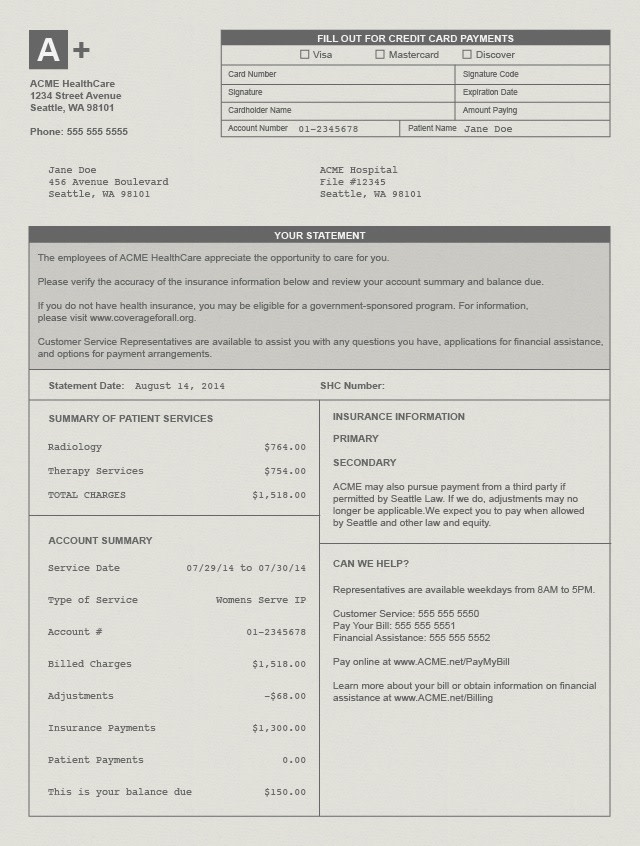
- Argument Appointment: The date your healthcare provider printed the bill.
- Account Number: This is your own unique business relationship number. If you have questions regarding your bills and residue, yous need to provide this number when contacting your healthcare provider's billing office. Business relationship numbers are also typically used when you pay for a bill online.
- Service Date: Your bill includes a column list the dates you received each medical service.
- Description: This is a short phrase that explains the service or supplies yous received.
- Charges: This is the total toll of the services or supplies yous received before insurance has been factored in.
- Billed Charges: This is the total amount charged directly to either you or your insurance provider.
- Adjustment: This is the amount the healthcare provider has agreed not to accuse.
- Insurance Payments: The amount your health insurance provider has already paid.
- Patient Payments: The amount yous are responsible to pay.
- Residual/ Corporeality Due: The amount currently owed the healthcare provider.
- Payable to: This is the organization you should address cheque payments to.
You lot may as well run across a "service code" listed on your bill. Healthcare providers use a standardized Current Procedural Terminology (CPT) or Healthcare Common Procedure Coding System (HCPCS) to identify the exact services and supplies you lot received during your appointment. Notation: Coding protocol is used internally and may not be included on your bill.
What is an Explanation of Benefits (EOB)?
An EOB is a document sent to insured individuals after a claim has been submitted by a healthcare provider. Information technology explains what medical treatments and services the patient'southward health insurance company agreed to pay for and what treatments/services (if whatever) the patient is responsible for paying. EOB stands for caption of benefits. Information technology is not the aforementioned as a medical nib, although information technology may look similar and show a residuum due. When the EOB indicates that money is nonetheless owed to the doctor or dentist who provided care, patients tin can await a separate bill to be sent from the medico or dentist'due south part. In this instance, payment should be made directly to the practitioner, not to the insurance company who sent the EOB. The purpose of EOBs is to proceed consumers informed of their healthcare costs and expenditures. It too offers insured customers a chance to double-bank check that services are billed correctly.
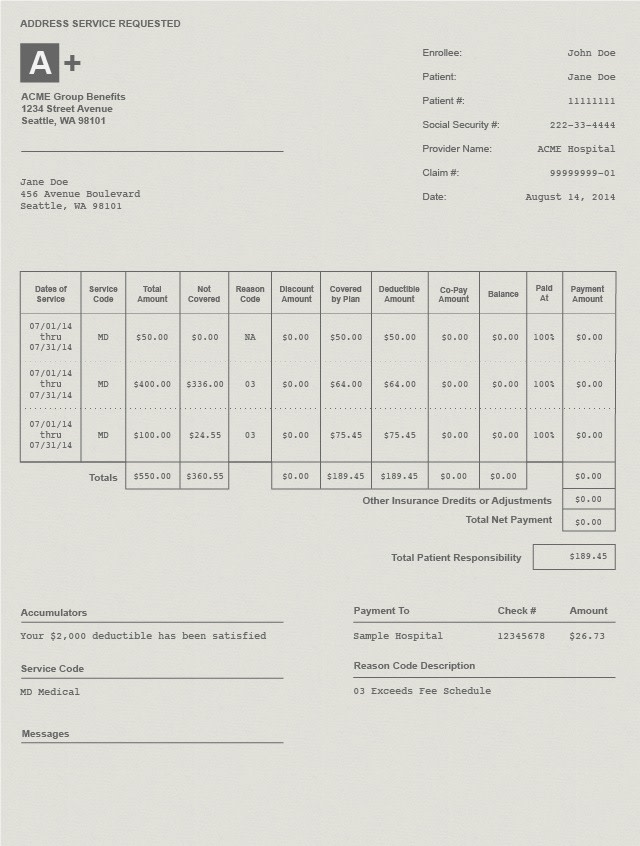
- Member Information: This shows the health insurance member's total name and ID number.
- Patient Account Number: This is the unique identification number used by your healthcare provider to track your account.
- Provider Name: The proper name of the hospital, physicians' office, or healthcare professional person you visited during your appointment.
- Claim Number: This unique identification number is used by your insurance provider to rail your account.
- Date of service: The date yous received the medical services, procedures, or supplies.
- Service Code: This identifies the specific services, procedures, or supplies you lot received from a healthcare provider.
- Total Amount: This dollar amount shows the full cost of the procedures, services, or supplies.
- Not Covered: This is the amount your health insurance does not cover. Yous are responsible for this amount.
- Reason Code Description: This code provides the reason(due south) why your insurer did not cover a charge.
- Covered past Plan: This is the total amount your wellness insurance provider has saved you.
- Deductibles and Copayments: Adjustments added based on the deductible and copay features of your insurance plan.
- Total Net Payment: This includes the total dollar amount your insurance visitor has paid to your healthcare provider.
- Full Patient Responsibility: This is the total amount you owe your healthcare provider.
- Checks Issued: This section gives y'all a detailed record of the payment transactions from your insurer to your healthcare provider. These lists by and large contain the payee's name, cheque number, and cheque corporeality.
Dealing With Billing Errors
Since medical billing processes involve several parties – you, your insurer, and your healthcare provider – mistakes can and do happen. A medical coder might take inaccurately described your care history with an inaccurate code, a medical biller might have mistyped a value, or a claims adjuster might have applied the wrong plan information to your claim. Regardless of the reason backside this error, it is important for yous every bit a patient to monitor your bills and EOB forms. If you notice charges that await out of identify, do not hesitate to contact your insurers and/or healthcare providers to dispute the error.
Identifying Errors
- Compare estimates to your terminal bill: Before your appointment, contact the healthcare provider and ask to exist given the billing lawmaking and cost. Side by side, contact your health insurance provider to make sure the procedure is covered by your plan and obtain an approximate of how much you will demand to pay for the procedure. If your estimated full is very different from your balance due later the appointment, there may be a billing error.
- Create a list of charges: Create a tape of all the medical services and supplies you received, along with their corresponding charges. This can aid y'all identify an incorrect charge in the futurity.
- Duplicate charges: If you notice the same accuse listed twice, information technology is probable that an error occurred during data entry.
- Beware of upcoding: Upcoding is the criminal act of fraudulently reporting an incorrect diagnosis in order to profit. A disreputable healthcare provider might use upcoding so information technology receives a big payment from you or your insurance company. If a procedure description or code seems to include services you did not agree to, it could be a grade of upcoding.
- Check identifying information: Make sure your proper name and identification numbers are correct. Mistakes in identification could lead to insurance coverage discrepancies.
Disputing Charges
- Contact your healthcare provider'south billing office: Speak to your healthcare provider near bill inaccuracies. If they made an mistake during the claims process, they should be able to correct information technology. Take note of the billing representative, the appointment, and time of your phone call.
- Call your insurer: If you are unable to resolve the fault with your healthcare provider, contact your insurer nigh the disputed charge. They tin work with yous to file a formal appeal to dispute a accuse. They can also examine your bill for red flags that could indicate fraudulent activity committed past the healthcare provider.
- Contact a credit-reporting bureau: Make certain your disputed bills do non touch your credit score. As you dispute a charge, your healthcare provider might mark the bill as overdue, which can impact your credit score. Your credit agency should be able to address credit score issues if yous are still disputing a charge.
- Credit reporting agencies:
- Experian
- TransUnion
- Equifax
- Credit reporting agencies:
- Submitting credit complaints: Federal Trade Commission Complaint Banana
Above all, remember to non be afraid to ask questions when at the hospital or doc's role; it is important to properly grasp what is covered by your insurance. Maintain a record of your medical bills and keep an eye out for errors and discrepancies.
What To Do When You Get Billed Twice By Health Services,
Source: https://www.medicalbillingandcoding.org/health-insurance-guide/understanding-medical-bills/
Posted by: harrellgare1973.blogspot.com


0 Response to "What To Do When You Get Billed Twice By Health Services"
Post a Comment